Women in midlife—roughly between ages 40–55—often experience a perfect storm: fluctuations in estrogen and progesterone, increased stress, and mounting inflammation. These factors don’t just affect how you feel; they can disrupt sleep, bone health, metabolism, and emotional resilience.
Here’s a deep dive into how hormones and inflammation interact during this phase, and the tools you can use to navigate this stage with more balance and insight.
Why Midlife Is a Turning Point
As estrogen and progesterone decline, inflammation becomes more noticeable—and more persistent. Estrogen has anti-inflammatory effects, protecting joints, blood vessels, brain function, and skin. As levels drop, inflammatory markers like CRP and IL-6 tend to rise.
Add in life stressors—like career shifts or caregiving—and immune regulation can feel like it’s slipping away.
Common Signs in Midlife
-
Stiff, achy joints and slower recovery
-
Weight gain (especially around the waist)
-
Disrupted sleep and increased nighttime cortisol
-
Mood swings, irritability, or low energy
-
Sensitive digestion and food cravings
These symptoms aren't inevitable—but they often come up because hormones and inflammation are talking to each other.
The Hormone‑Inflammation Feedback Loop
-
Hormone shifts lower protective estrogen, which increases sensitivity to inflammatory triggers.
-
Inflammation affects cortisol—altered cortisol regulation further disrupts sleep and hormone balance.
-
Sleep disruption increases insulin resistance, which feeds inflammation and hormonal imbalance further.
It’s a cycle—but one you can influence.
Tools to Support Hormonal Balance and Reduce Inflammation
1. Track and Sync
Wearables like the Ōura Ring help correlate cycle phase with changes in sleep, inflammation, or energy. Recognizing patterns can empower you to shift workload, stress support, or recovery routines on demand.
2. Targeted Supplements
-
Omega-3s and curcumin address inflammation directly.
-
Magnesium supports sleep and lowers cortisol.
-
Adaptogens like ashwagandha or rhodiola help stabilize stress hormones.
Remain consistent with mid-cycle hormonal changes and understand interactions.
3. Infrared and Cold Therapy
-
Evening infrared saunas support blood pressure, circulation, and heat shock protein activation—helpful during estrogen shifts.
-
Cold plunges can help reset the stress response during high-tension phases, but should be balanced with sauna if you’re hormonally sensitive.
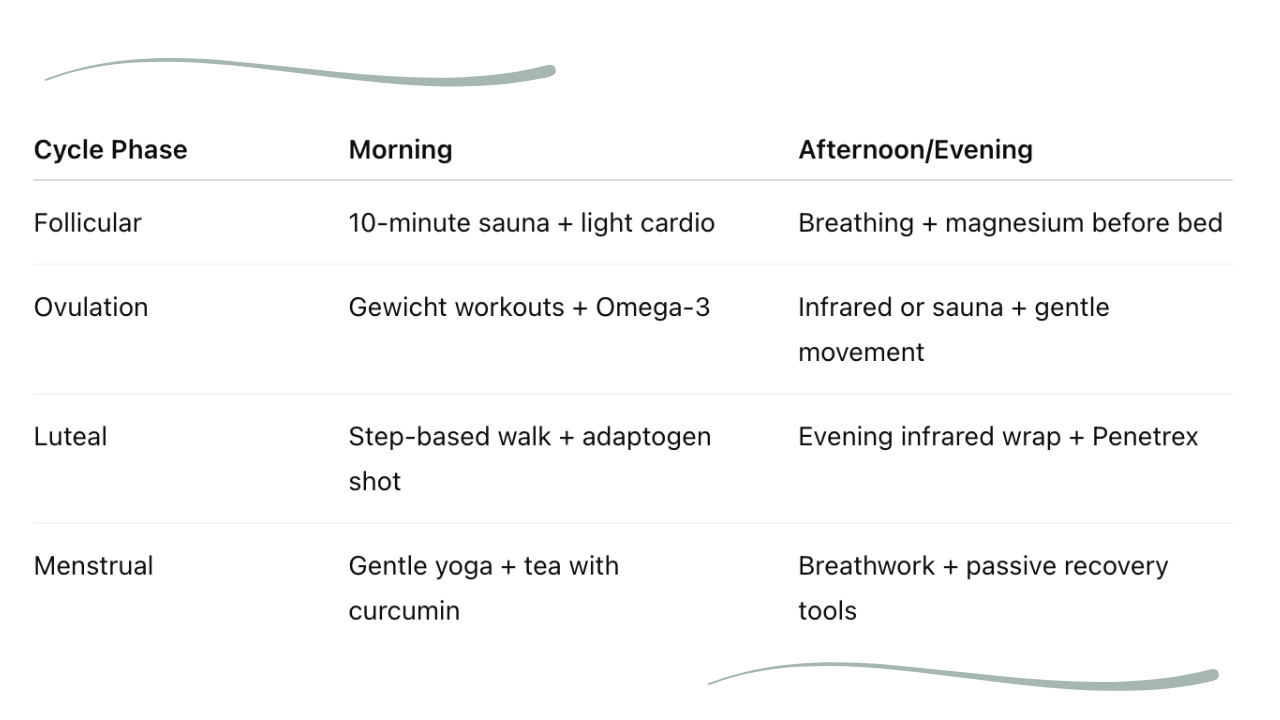
4. Cycle-Synced Movement
-
Follicular phase: energy is high—lean into cardiovascular or resistance training.
-
Ovulatory phase: focus on performance but maintain recovery.
-
Luteal phase: shift toward restorative movement.
-
Menstrual phase: prioritize rest, gentle stretching, and passive recovery.
Practical Routine in Real Life
FAQs & Common Concerns
“Is hormone replacement necessary?”
Not always—but if symptoms like bone loss or severe mood shifts appear, it’s worth discussing with your provider while also supporting recovery tools.
“How do I know if I’m inflamed?”
Look for symptoms combined with wearables data (e.g., elevated resting heart rate) or labwork (CRP). Tracking across the cycle helps pinpoint trends.
“Can’t I just rely on food?”
Nutrition is crucial, but midlife changes often require multidimensional support—lighting, movement, recovery tools, lifestyle, and sometimes supplements.
Final Takeaway
Midlife hormones and inflammation are deeply connected—and each informs the other. That doesn’t make symptoms inevitable—it just means there's more data to use, and more tools that can help.
By syncing tools to your cycle, you’re not fighting biology. You’re working with it. And that’s exactly how sustainable change is created.
Explore our curated tools for hormone support, from cycle-tracking wearables to infrared wraps that soothe your system—designed for women who want grounded, science-based solutions as they age.




